Estrogen is the female hormone that’s been used to manage menopause symptoms like hot flashes, night sweats, and vaginal dryness. However, the use of estrogen has also been widely debated because it is linked to breast cancer and other health risks. So, how can you tell if the information you read about estrogen safety is credible?
While short-term use of estrogen can offer benefits in managing menopausal symptoms, many studies have shown that long-term use of hormones is associated with increased breast cancer risk. The most influential paper was published in JAMA in 2002 by the Women’s Health Initiative (WHI) study (1).
The Women’s Health Initiative (WHI) Clinical Study
WHI is one of the largest, longest, and most comprehensive studies focused on women’s health. It was launched in 1991 by the National Institutes of Health (NIH) to address significant health issues affecting women. Long-term estrogen + progestin therapy was shown to increase the risk of breast cancer, stroke, heart disease, and blood clots, and a moderately decreased risk in colon cancer and hip fractures.
The highly increased blood clotting risk in older women is particularly concerning because clots can block blood flow to vital organs, potentially leading to a heart attack, stroke, pulmonary embolism (a blood clot in the lungs), deep vein thrombosis (DVT), or even kidney failure. The estrogen-only WHI arm did not show the same increase in breast cancer risk, but it also had different risks, including increased stroke risk and findings that apply only to women who had a hysterectomy.
The WHI study is still ongoing. To date, over 2,500 papers have been published based on the WHI study, offering a more in-depth exploration of specific topics. A 2024 review in JAMA provides an updated, comprehensive summary of the hormone-therapy trial findings (2). It reinforces that WHI evidence does not support menopausal hormone therapy (MHT) for chronic disease prevention.
Historical Evidence
When the Women's Health Initiative (WHI) released data in 2002 linking HRT to breast cancer, many women in developed countries stopped the therapy. This was followed by a sharp and immediate decline in breast cancer incidence in those same countries, a trend not seen in developing nations where HRT use was low (3).
Trends in hormone replacement therapy (HRT) use (all formulations) over time in the USA.
Molecular Evidence Supports WHI Findings
A 2023 Harvard study published in Nature (4) provided molecular evidence. This evidence supports the WHI epidemiological findings by showing how estrogen may drive tumor development at the molecular level.
This study explains how estrogen can contribute to the development of breast cancer in susceptible women. When estrogen binds to its receptor in breast cells, it can cause DNA damage, altering the structure of chromosomes. These changes, known as translocations, can rearrange pieces of DNA from different chromosomes, leading to the overproduction of certain cancer-causing genes. Essentially, estrogen doesn't just fuel the growth of breast cancer cells, but it may actually help create the genetic changes that turn healthy cells into cancerous ones.

The study shows that estrogen's role in breast cancer isn’t just about making existing cancer cells grow faster, but also about triggering genetic changes that lead to cancer in the first place. This is important because it helps us understand why hormone therapy and prolonged estrogen exposure may increase the risk of developing breast cancer, especially in women with certain genetic traits.
Mechanistic studies like this help explain how estrogen-related cancers may develop, strengthening long-term observational findings.
Why Conflicting Studies Exist?
Following the publication of the WHI study report, sales of estrogen declined. In response, several industry-funded studies have reported findings that differ from those of the WHI. Because funding sources can influence study design, interpretation, or statistical framing, these results should be carefully evaluated. The WHI study is robust, with molecular evidence to support its findings. How can many conflicting findings challenge solid science?
Tactics Used by Commercial Interests
History shows that when strong scientific evidence threatens profits, industries may fund research to create confusion rather than clarity.
A well-known example is tobacco. Today, it is undeniable that smoking causes lung cancer, based on decades of data showing that most lung cancer patients have a history of smoking. However, this evidence threatened the tobacco industry’s profits. In response, tobacco companies funded “independent” research that claimed smoking was not harmful or that secondhand smoke posed little risk. These studies contradicted overwhelming evidence and were used to confuse the public, delay regulation, and undermine independent research linking smoking to cancer and heart disease.
Tactics used by the tobacco industry included:
- Funding biased research presented as independent to downplay health risks
- Creating doubt by publishing conflicting studies despite clear evidence
- Promoting “safer” products such as low-tar cigarettes, which were no less harmful
- Misleading advertising suggesting medical endorsement of smoking
- Downplaying secondhand smoke risks
- Discrediting independent researchers who reported harm
- Delaying regulation by challenging public health findings
- Framing regulation as a freedom issue, arguing that smoking was a personal choice
These tactics allowed the tobacco industry to protect profits and delay public health action for decades.
Similar Tactics Used in Estrogen Promotion
Industries that produce estrogen have used similar strategies. By funding favorable studies and selectively publishing results, they have influenced public opinion and medical practice.
Common tactics used by drug companies include:
- Funding biased research that minimizes risks such as breast cancer, heart disease, and stroke
- Influencing medical professionals through sponsored conferences and education
- Marketing estrogen as “safe” or “protective”, while downplaying long-term risks
- Promoting low-dose or “bioidentical” estrogen as safer alternatives despite similar risks
- Targeting vulnerable groups, including breast cancer survivors
- Using misleading advertisements that focus on short-term symptom relief
- Discrediting independent studies, including the WHI study
- Leveraging influential doctors and public figures to build trust
After the WHI study showed that long-term hormone therapy increased breast cancer risk, drug companies funded new studies claiming estrogen was safe—even for breast cancer survivors. These company-sponsored studies dismissed earlier findings as “outdated” and encouraged the public to accept the new conclusions.
The Core Question
These newer studies often appear scientifically sound. This raises an important question for women: How can the public know what to trust—the independent WHI findings or studies funded by companies with financial interests? Understanding the role of funding and incentives is critical when interpreting medical research, especially for treatments intended for long-term use.
How to Identify Credible Information?
For a study on a product’s cancer risk, two factors are critical: the duration of the study and the financial sponsorship.
- Duration: Short-term studies can’t provide accurate information on cancer risks. The example of the 4-year study on college students that showed smoking did not cause lung cancer is not credible, because lung cancer may take decades to develop, just like breast cancer risk.
- Sponsorship: Studies sponsored by companies that sell estrogen may have a conflict of interest. For instance, a study (10) that concluded that vaginal estrogen cream is safe for breast cancer survivors is sponsored by a company that sells vaginal estrogen cream. Industry funding may influence study design, interpretation, or conclusions, which need careful evaluation. In fact, some vaginal formulations show significant systemic absorption, suggesting that they may not always offer a clear safety advantage over oral estrogen (11, 12), particularly in breast cancer survivors.
In contrast, the WHI study was publicly funded, followed participants for over 30 years, and has no commercial interests. Therefore, the WHI report is more credible and not "outdated."
Trust Science
Recently, Harvard researchers published a scientific paper in Nature (3), discovering the potential role of estrogen in the development of breast cancer at the molecular level. This article provides solid evidence that supports the findings of the WHI study (1, 2). Articles published in Nature are highly credible due to their rigorous peer-review process. As one of the most respected scientific journals, Nature is known for publishing groundbreaking research. Nature’s world recognition and commitment to science ensure that its articles are reliable.
Trust Your Common Sense
Additionally, you can use your common sense to find out the answer. Today, there are 5.5 million women with a history of estrogen-sensitive cancers (4.3 million breast, 0.95 million uterine, and 0.25 million ovarian) living in the United States. You may find them in your family, among relatives, and in your neighborhood. By talking to them, you may find that many of them do not have a family history of cancer, but may have a history of taking hormone replacement therapy. Their experiences may provide additional perspective on potential risks.
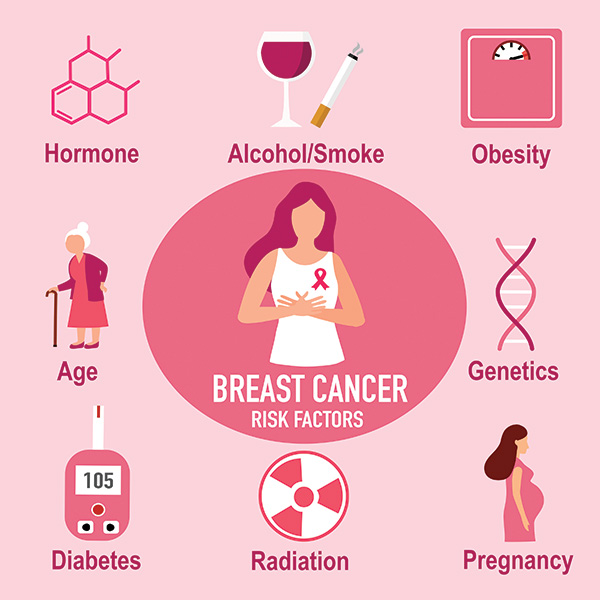
Hormones are not the only risk factor for breast cancer. There are other factors, such as alcohol, smoking, obesity, age, genetics, diabetes, radiation, and pregnancy. However, having other risk factors does not exclude hormones from being a risk factor. Unlike genetics and aging, the risk of cancer due to hormones is avoidable.
Although personal stories cannot replace scientific data, speaking with women who have had estrogen-sensitive cancers may help improve your understanding of the potential cancer risk of hormones.
Trust Independent Scientists
A group of independent scientists in the field of cancer research, not related to drug companies, has voiced their concerns about the cancer risk of estrogen. They wrote a letter to the FDA (13). In the letter, they urge the FDA not to remove Boxed Warnings from vaginal estrogen products without proper scientific review. They emphasize that:
- Most vaginal estrogen trials last fewer than 12 weeks.
- No randomized study of estrogen has gone beyond one year.
- Long-term safety of estrogen remains unknown.
They request that the FDA hold a formal advisory committee meeting, with full transparency and public participation, before making any changes to hormone therapy labeling to ensure patient safety.
A recent American Family Physician article (14) also highlights the limitations of menopausal hormone therapy.
Conclusion
Long-term, well-designed, and independent studies like WHI offer the most credible information on hormone therapy risks. Short-term or industry-sponsored studies should be interpreted cautiously, especially when evaluating potential cancer risks. When considering hormone therapy, rely on long-term, independent research rather than short-term or commercially funded studies.
Ask:
- How long did the study last, and does it track long-term risks or just short-term effects?
- Who funded the study, and is there a potential conflict of interest (e.g., funding by a company that sells estrogen products)?
- Does the study explain how estrogen may trigger cancer risk over time?
- Is the study based on new, credible research or outdated data?
- Does the paper offer a balanced view of estrogen’s risks and benefits?
- Does it discuss how individual factors, such as age, family history, and therapy duration, affect safety?
Hormone therapy can be helpful for short-term relief from menopause symptoms, like hot flashes, night sweats, and vaginal dryness, but it should always be used with guidance from a healthcare provider. The WHI study showed that long-term estrogen use to manage conditions like menopause carries serious risks.
Menopause is a natural life stage, not a disease, according to the World Health Organization (WHO) (15). Using estrogen long-term for a non-disease condition is overmedication, where the risks outweigh the benefits. Safer alternatives to estrogen should be considered for better health.
Be cautious when reading information that seems too good to be true. Ask the right questions, look for balanced evidence, and always be mindful of the sponsor behind the research. When making decisions about estrogen therapy, knowledge is power. Don’t let misleading or biased information shape your health decisions.
Reference:
1. Writing Group for the Women's Health Initiative Investigators. Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results From the Women's Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321–333. doi:10.1001/jama.288.3.321. https://jamanetwork.com/journals/jama/fullarticle/195120
2. Manson JE, Hsia J, Johnson KC, et al. “The Women’s Health Initiative Randomized Trials and Clinical Practice: A Review.” JAMA. 2024;331(20):1748-1760. https://jamanetwork.com/journals/jama/article-abstract/2818206
3. Zbuk K, Anand SS. Declining incidence of breast cancer after decreased use of hormone-replacement therapy: magnitude and time lags in different countries. J Epidemiol Community Health 2012;66:1-7. https://jech.bmj.com/content/66/1/1
4. Lee, J.JK., Jung, Y.L., Cheong, TC. et al. ERα-associated translocations underlie oncogene amplifications in breast cancer. Nature 618, 1024–1032 (2023). https://doi.org/10.1038/s41586-023-06057-w
5. McGarity JB, Wagner WE. Inventing Conflicts of Interest: A History of Tobacco Industry Tactics. American Journal of Public Health. 2008;98(4):623–632. DOI: 10.2105/AJPH.2007.117980. PMC
6. Bero LA, Glantz SA, Hong MK. “Commercial Tobacco and Nicotine Industry‑Funded Research Has a Significant Effect on the Evidence Base: A Meta‑Review.” Nicotine & Tobacco Research. 2024;26(8):963‑971. DOI:10.1093/ntr/ntad056. OUP Academic
7. “Influencing Science Case Studies – Tobacco Tactics.” TobaccoTactics.org, University of Bath. 2024. Tobacco Tactics
8. “The Smokescreen of the Tobacco Industry’s Use of Science.” UICC (Union for International Cancer Control) News. 2020. UICC
9. “Dead Ends – The Tobacco Industry’s Quest for a ‘Safe’ Combustible.” Global Tobacco Harm Reduction Network briefing paper. 2024.
10. FDA. FACT SHEET: FDA Initiates Removal of “Black Box” Warnings from Menopausal Hormone Replacement Therapy Products. https://www.fda.gov/news-events/press-announcements/hhs-advances-womens-health-removes-misleading-fda-warnings-hormone-replacement-therapy
11. Beste, Mary E. et al. Vaginal estrogen use in breast cancer survivors: a systematic review and meta-analysis of recurrence and mortality risk. American Journal of Obstetrics & Gynecology, 232 (3), 262 - 270.e1. https://www.ajog.org/article/S0002-9378(24)01126-8/fulltext
12. Martin PL, Yen SS, Burnier AM, Hermann H. Systemic absorption and sustained effects of vaginal estrogen creams. JAMA. 1979 Dec 14;242(24):2699-700. PMID: 228093. https://jamanetwork.com/journals/jama/article-abstract/367863
13. Moegele M, Buchholz S, Seitz S, Ortmann O. Vaginal estrogen therapy in postmenopausal breast cancer patients treated with aromatase inhibitors. Arch Gynecol Obstet. 2012 May;285(5):1397-402. doi: 10.1007/s00404-011-2181-6. Epub 2012 Jan 3. PMID: 22212649. https://pubmed.ncbi.nlm.nih.gov/22212649/
14. https://georgetown.app.box.com/s/mbcors2rmrrsumyh8ikiv7ct869ulhlp
15. Fugh-Berman A, Mintzes B. Menopausal Hormone Therapy: Limited Benefits, Significant Harms. Am Fam Physician. 2025 Jul;112(1):15-16. PMID: 40736486. https://www.aafp.org/pubs/afp/issues/2025/0700/editorials-menopausal-hormone-therapy.pdf
16. WHO. Menopause. https://www.who.int/news-room/fact-sheets/detail/menopause
