Many studies have shown that hormone therapies after menopause are associated with increased breast cancer risk. The most influential paper was published in JAMA in 2002 by the Women’s Health Initiative (WHI) study (1).
The Women’s Health Initiative (WHI) Clinical Study
WHI is one of the largest, longest, and most comprehensive studies focused on women’s health. It was launched in 1991 by the National Institutes of Health (NIH) to address major health issues that affect women. Long-term estrogen + progestin therapy was shown to increase breast cancer risk. The estrogen-only WHI arm did not show the same increase in breast cancer risk, but it also had different limitations and risks, including increased stroke risk and findings that apply only to women who had hysterectomy.
Moleucular Evidence Supports WHI Findings
A 2023 Harvard study published in Nature (2) provided molecular evidence. This evidence supports older epidemiological findings by showing how estrogen may drive tumor development at the molecular level. Mechanistic studies like this help explain how estrogen-related cancers may develop, strengthening long-term observational findings.
Why Conflicting Studies Exist?
Following the publication of the WHI study report, sales of estrogen declined. In response, several industry-funded studies have reported findings that differ from those of the WHI. Because funding sources can influence study design, interpretation, or statistical framing, these results should be carefully evaluated. The WHI study is solid, and it has molecular evidence to support it. How could the solid finding be challenged by many conflicting studies?
Simple Tactics Used by Commercial Interests
Let’s consider an example to illustrate how companies may use simple tactics to generate contradictory findings.
Today, it is widely accepted that smoking causes lung cancer. This conclusion is based on decades of data showing that most lung cancer patients have a history of smoking. However, this knowledge harms the profits of the tobacco industry. To increase cigarette sales, tobacco companies might sponsor studies targeting college students for a four-year duration. The study would find that none of the smokers developed lung cancer. Such a study could be used to claim that previous studies linking smoking to lung cancer are outdated. New evidence shows that smoking does not cause lung cancer.
Likewise, after the WHI study reported that estrogen increased the risk for breast cancer, drug companies sponsored similar studies. These studies showed that estrogen did not increase the risk of breast cancer and is safe for women, even safe for breast cancer survivors who are highly sensitive to estrogen. As a result, the company-sponsored researchers claimed that the previous studies were outdated. People should accept their new findings.
Their study designs look logical, and their conclusions appear scientifically sound. So how can regular women know what to trust: The WHI report or the new data from drug company-sponsored studies?
How to Identify Credible Information?
For a study on a product’s cancer risk, two factors are critical: the duration of the study and the financial sponsorship.
- Duration: Short-term studies can’t provide accurate information on cancer risks. The example of the 4-year study on college students that showed smoking did not cause lung cancer is not credible, because lung cancer may take decades to develop, just like breast cancer risk.
- Sponsorship: Studies sponsored by companies that sell estrogen may have a conflict of interest. For instance, a study that concluded that vaginal estrogen cream is safe for breast cancer survivors is sponsored by a company that sells vaginal estrogen cream. Industry funding may influence study design, interpretation, or conclusions, which need careful evaluation. In fact, some vaginal formulations show significant systemic absorption, suggesting that they may not always offer a clear safety advantage over oral estrogen (3, 4), particularly in breast cancer survivors.
In contrast, the WHI study was publicly funded, followed participants for over 30 years, and has no commercial interests. Therefore, the WHI report is more credible and not "outdated."
Trust Science
Recently, Harvard researchers published a scientific paper in Nature (2), discovering the potential role of estrogen in the development of breast cancer at the molecular level. This article provides solid evidence that supports the findings of the WHI study (1). Articles published in Nature are highly credible due to their rigorous peer-review process. As one of the most respected scientific journals, Nature is known for publishing groundbreaking research. Nature’s world recognition and commitment to science ensure that its articles are reliable.
Trust Your Common Sense
Additionally, you can use your common sense to find out the answer. Today, there are 5.5 million women with a history of estrogen-sensitive cancers (4.3 million breast, 0.95 million uterine, and 0.25 million ovarian) living in the United States. You may find them in your family, among relatives, and in your neighborhood. By talking to them, you may find that many of them do not have a family history of cancer, but may have a history of taking hormone replacement therapy. Their experiences may provide additional perspective on potential risks.
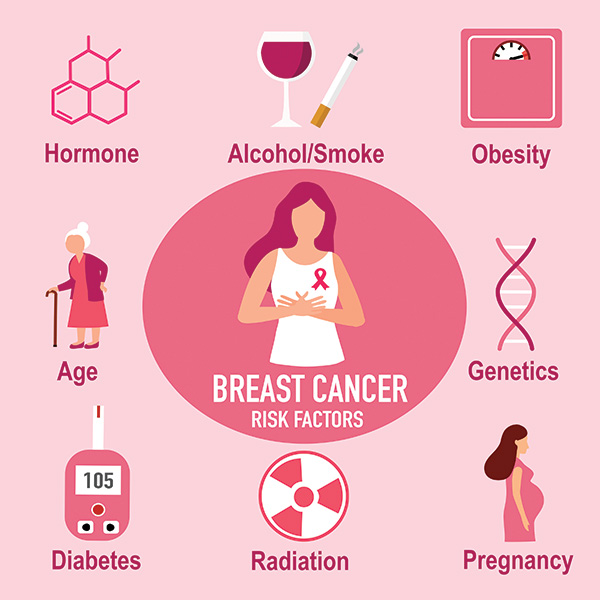
Hormones are not the only risk factor for breast cancer. There are other factors, such as alcohol, smoking, obesity, age, genetics, diabetes, radiation, and pregnancy. However, having other risk factors does not exclude hormones from being a risk factor. Unlike genetics and aging, the risk of cancer due to hormones is avoidable.
Although personal stories cannot replace scientific data, speaking with women who have had estrogen-sensitive cancers may help improve your understanding of the potential cancer risk of hormones.
Trust Independent Scientists
A group of independent scientists in the field of cancer research, not related to drug companies, has voiced their concerns about the cancer risk of estrogen. They wrote a letter to the FDA (5). In the letter, they urge the FDA not to remove Boxed Warnings from vaginal estrogen products without proper scientific review. They emphasize that:
- Most vaginal estrogen trials last fewer than 12 weeks.
- No randomized study of estrogen has gone beyond one year.
- Long-term safety of estrogen remains unknown.
They request that the FDA hold a formal advisory committee meeting, with full transparency and public participation, before making any changes to hormone therapy labeling to ensure patient safety.
A recent American Family Physician article (6) also highlights the limitations of menopausal hormone therapy.
Conclusion
Long-term, well-designed, and independent studies like WHI offer the most credible information on hormone therapy risks. Short-term or industry-sponsored studies should be interpreted cautiously, especially when evaluating potential cancer risks. When evaluating hormone therapy, rely on long-term, independent research rather than short-term or commercially funded studies.
Reference:
1. Writing Group for the Women's Health Initiative Investigators. Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results From the Women's Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321–333. doi:10.1001/jama.288.3.321. https://jamanetwork.com/journals/jama/fullarticle/195120
2. Lee, J.JK., Jung, Y.L., Cheong, TC. et al. ERα-associated translocations underlie oncogene amplifications in breast cancer. Nature 618, 1024–1032 (2023). https://doi.org/10.1038/s41586-023-06057-w
3. Martin PL, Yen SS, Burnier AM, Hermann H. Systemic absorption and sustained effects of vaginal estrogen creams. JAMA. 1979 Dec 14;242(24):2699-700. PMID: 228093. https://jamanetwork.com/journals/jama/article-abstract/367863
4. Moegele M, Buchholz S, Seitz S, Ortmann O. Vaginal estrogen therapy in postmenopausal breast cancer patients treated with aromatase inhibitors. Arch Gynecol Obstet. 2012 May;285(5):1397-402. doi: 10.1007/s00404-011-2181-6. Epub 2012 Jan 3. PMID: 22212649. https://pubmed.ncbi.nlm.nih.gov/22212649/
6. Fugh-Berman A, Mintzes B. Menopausal Hormone Therapy: Limited Benefits, Significant Harms. Am Fam Physician. 2025 Jul;112(1):15-16. PMID: 40736486. https://www.aafp.org/pubs/afp/issues/2025/0700/editorials-menopausal-hormone-therapy.pdf
